Anal Tampon vs. Conventional Gauze: A Breakthrough in Post-Hemorrhoidectomy Bleeding Control

Anorectal disorders significantly impact an individual’s quality of life, affecting the anus and rectum. Among the most common anal and rectal disorders are hemorrhoids, anal fissures, and anal fistulas [1]. Of these, hemorrhoids are the most prevalent, affecting approximately 10 million people each year. In fact, more than 50% of the U.S. population over the age of 50 has experienced hemorrhoids at some point in their lives [2].
What Are Hemorrhoids?
Hemorrhoids are normal submucosal venous structures in the lower rectum and anal canal that play a role in maintaining faecal continence. However, when they become swollen or inflamed, they can cause discomfort, itching, pain, and rectal bleeding.
Types of Hemorrhoids
Hemorrhoids are categorized based on their location relative to the dentate line:
- Internal Hemorrhoids: Located above the dentate line, these hemorrhoids are often painless but may cause bleeding during bowel movements.
- External Hemorrhoids: Found below the dentate line, these can be painful, particularly if they become thrombosed.
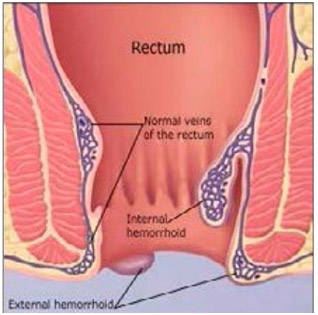 Fig.1: An illustration of internal and external hemorrhoids [2].
Fig.1: An illustration of internal and external hemorrhoids [2].
The Need for Modern Surgical Solutions
While conservative treatments such as dietary changes, increased fibre intake, and topical medications can help manage mild cases, surgical intervention remains the most effective approach for severe or persistent hemorrhoids. However, conventional surgical practices, such as open and closed hemorrhoidectomies, are associated with significant post-operative pain, bleeding, and longer recovery times [3]. This underscores the necessity of adopting modern surgical solutions to enhance patient care.
Modern Advancements in Hemorrhoid Surgery
Traditional hemorrhoidectomy techniques, including Milligan-Morgan and Ferguson procedures, often lead to prolonged healing and post-surgical complications. In contrast, modern approaches such as stapled hemorrhoidopexy (SH) and partial stapled hemorrhoidopexy (PSH) offer superior patient outcomes by reducing pain, lowering the risk of bleeding, and ensuring quicker recovery [4, 5].
Furthermore, post-surgical care plays a crucial role in patient recovery. Conventional gauze packing, though widely used, presents multiple drawbacks, including increased pain, discomfort, and inadequate haemostasis. Additionally, it sheds fibres when cut and is prone to linting, leaving residual fibres in the wound after dressing removal [6]. This has led to the development of advanced haemostatic solutions like SURGISPON® Anal Tampon, designed to enhance recovery and improve surgical outcomes.
SURGISPON® Anal Tampon
For patients undergoing hemorrhoidectomy, SURGISPON® Anal Tampon serves as an advanced absorbable haemostatic gelatin sponge specifically developed for anorectal, vaginal, and rectal surgical procedures. It offers several advantages over conventional gauze, ensuring better post-operative care and patient comfort.
 WHY USE SURGISPON® Anal Tampon OVER CONVENTIONAL GAUZE??
WHY USE SURGISPON® Anal Tampon OVER CONVENTIONAL GAUZE??
| Characteristic | SURGISPON® Anal Tampon | Conventional Gauze |
| Composition |
|
|
| Blood Absorption | High absorption capacity (absorbs 45 times its weight) | Absorbs significantly less blood |
| Design | Cylindrical shape with a hollow centre (80×30 mm) | Gauze is manually molded into an anal canal |
| Clotting Mechanism | Aids in clotting by conforming to the anal canal, applying pressure to the bleeding site, and trapping platelets to form a stable fibrin clot | Doesn’t aid in clotting process |
| Insertion | Painless insertion, reducing post-operative pain | Causes high discomfort and pain during insertion |
| Removal | No need for removal—liquefies and is expelled naturally during the first bowel movement | Must be removed manually, causing discomfort |
| Non-Adherent Properties | Prevents tissue disruption by not adhering to the wound | May adhere to the wound, leading to tissue disruption |
| Flatus Drain | Includes an opening for flatus drain, preventing gaseous obstruction | May cause gaseous obstruction |
| Time to Haemostasis (TTH) | 2 to 5 min | More than 10 to 15 min |
| Complications | No reported complications | Risk of bleeding, pain, urinary retention and infection |
| Use as a carrier/co-adjuvant | pH-neutral, can be used dry or can be combined with analgesics, antibiotics, and other medications | Can’t be used as co-adjuvant |
Clinical Evidence Supporting Gelatin Sponge Use Over Conventional Gauze
A retrospective study compared the effectiveness of an absorbable gelatin sponge with epinephrine-soaked gauze in post-hemorrhoid surgery care for 291 patients. The study found that patients using gelatin sponges experienced:
- Significant pain reduction: Lower pain scores from 8 hours to 2 days post-surgery compared to those using epinephrine-soaked gauze.
- Enhanced comfort: A more comfortable post-surgical experience without compromising recovery outcomes.
Although both groups had similar overall recovery timelines, the gelatin sponge demonstrated superior pain relief and patient comfort, reinforcing its value as a reliable and effective choice for postoperative care [7].
Bridging the Gap: Encouraging Doctors to Adopt Modern Surgical Practices
Despite the availability of advanced surgical solutions, many practitioners continue to rely on conventional methods due to a lack of awareness or resistance to change. It is essential to highlight the limitations of outdated techniques and emphasize the benefits of modern innovations in hemorrhoid management. By integrating advanced hemostatic dressings like SURGISPON® Anal Tampon, healthcare professionals can significantly improve patient recovery, reduce complications, and enhance overall post-surgical care.
Conclusion
Traditional gauze packing, while widely used, presents multiple limitations that compromise patient comfort and recovery. The introduction of modern hemostatic solutions such as SURGISPON® Anal Tampon marks a significant step forward in hemorrhoid treatment. By shifting towards these advanced approaches, medical professionals can ensure better patient outcomes, reduce post-operative pain, and improve surgical efficiency. The time has come to embrace modern surgical solutions for enhanced patient care and recovery.
References
- https://www.kansashealthsystem.com/care/conditions/anorectal-disorders
- Foxx-Orenstein AE, Umar SB, Crowell MD. Common anorectal disorders. Gastroenterology & hepatology. 2014 May;10(5):294.
- Li J, Ma H, Wang Y, Lai L, Zhang X, Wang Y. Updates of surgical treatment in hemorrhoidal disease. Advanced Chinese Medicine. 2024 Jul;1(3):156-61.
- Yau KK, Chung CC, Chan ES, Li MK. Initial experience with stapled haemorrhoidectomy: A local report. Annals of the College of Surgeons of Hong Kong. 2002 Feb;6(1):8-11.
- Elshazly WG, Elros MA, Ali AS, Radwan AM. Randomized Controlled Trial to Compare Stapled Hemorrhoidopexy Plus Ligation AnopexyWith Stapled Hemorrhoidopexy for Managing Grade III and IV Hemorrhoidal Disease. Diseases of the Colon & Rectum. 2024 Jun 1;67(6):812-9.
- Jones VJ. The use of gauze: will it ever change?. International wound journal. 2006 Jul;3(2):79-88.
- Tsai KM, Kiu KT, Yen MH, Yen YC, Tam KW, Chang TC. Comparison the effect of gelatin sponge and epinephrine-soaked gauze for hemostasis and pain control after hemorrhoidal surgery. Scientific Reports. 2023 Oct 21;13(1):18010.