Transforming Bleeding Control in Cardiac Surgery with SURGISPON® Patch
Introduction
In cardiac surgery, effective bleeding control is crucial not only for procedural success but also for the patient’s recovery and long-term health. Hemorrhagic complications in open-heart surgeries pose significant risks, with incidence rates ranging from 5-9% – and severe cases potentially reaching 16%. Blood transfusions, though often necessary, come with risks like adverse effects and pathogen transmission. Patients requiring reoperation due to bleeding face a three-fold increase in mortality risk. While surgical causes account for 66% of postoperative bleeding, 33% are due to coagulation disorders [1].
As we delve into the methods used in cardiac surgery for bleeding control, it’s important to first consider the traditional approaches that have formed the foundation of surgical practice for decades. These methods, while effective in many cases, highlight the need for advancements like the SURGISPON® Patch when faced with more complex challenges.
Traditional Methods for Controlling Bleeding
Bleeding control in cardiac surgery traditionally involves both systemic and local approaches, each with its own advantages and limitations.
Systemic Approaches
- Blood Transfusions: administration of red blood cells, platelets, plasma, and cryoprecipitate to provide essential clotting factors and volume support.
- Pro-Coagulant Medications: including anti-fibrinolytics like tranexamic acid and aminocaproic acid are used to prevent the breakdown of clots.
- Recombinant Factor VII: a synthetic clotting factor that promotes coagulation, particularly in severe bleeding cases.
Local Approaches
- Direct Surgical Techniques
- Suturing: closes bleeding vessels or tissues manually, though it’s time-consuming and requires precision.
- Vessel Ligation: ties off blood vessels to control bleeding but can be challenging in deep or small vessels.
- Electrocautery: uses electric current to coagulate blood and seal vessels quickly, though it risks tissue damage.
- Haemostatic Maneuvers
- Digital Pressure Application: using fingers (digits) to apply pressure to bleeding sites, providing immediate control. This method is not sustainable for long durations and may be ineffective in severe cases.
- Warm Saline Irrigation: flushes the area to manage bleeding sources, offering temporary hemostasis.
- Bone wax: composed of beeswax and paraffin or vaseline, frequently applied to control hemorrhage from the sternum by mechanically blocking the bone’s spongiosa [2, 3].
While traditional methods provide a strong foundation, they are not always sufficient, especially in cases involving complex coagulation disorders or extensive bleeding. To address these limitations, topical haemostatic agents have been developed, offering more targeted and effective solutions in challenging surgical scenarios.
Haemostatic Agents and Their Use in Cardiac Surgery
The development and use of haemostatic agents have significantly advanced the ability to control bleeding in cardiac surgery. These agents can be categorized based on their composition and mechanism of action.
- Haemostatic Agents with Active Mechanisms
These haemostatic agents work independently of coagulation mechanisms by introducing extrinsic clotting factors upon application, mimicking various stages of the coagulation process.
Examples
- Thrombin Sealants: Recothrom, Thrombogen, Thrombostat introduce thrombin directly to the wound site, promoting clot formation [4].
- Fibrin Sealants: Tisseel combines fibrinogen and thrombin to form a fibrin clot, mimicking the body’s natural clotting process [5].
- Fibrin Patches: TachoSil, TachoComb provide a physical matrix that supports clot formation [6].
- Autologous Fibrin and Thrombocyte Concentrates: Vivostat uses the patient’s own blood components to promote haemostasis [7].
- Gelatin-Thrombin Matrix Sealant: FLOGEL® and Floseal combine gelatin and thrombin to create a flexible, adherent matrix that promotes clot formation [8].
- Haemostatic Agents with inactive Mechanisms
These agents do not contain clotting factors and work by forming physical lattices that promote clot formation.
Examples
- Gelatin Sponges: Gelfoam, Gelaspon, provide a scaffold for clot formation [9].
- Microfibrillar Collagens: Avitene Flour MCH, Colgel, Helitene attract and activate platelets to form a clot [10, 11].
- Oxidized Regenerated Cellulose: Surgicel provides a physical barrier that aids in clot formation [12].
- Microporous Polysaccharide Hemispheres: Arista rapidly absorbs blood and concentrates clotting factors [13].
SURGISPON® Patch – A Crucial Solution in Cardiac Surgery
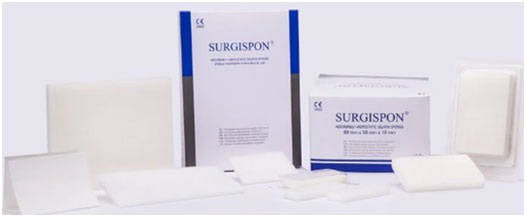
Aegis Lifesciences offers the SURGISPON® Patch, an absorbable hemostatic gelatin patch designed for cardiovascular applications including cardiac, great vessel, and peripheral vascular repair and reconstruction.
Benefits of SURGISPON® Patch
- Superior haemostasis: forms a stable clot, reducing the risk of excessive bleeding and minimizing blood transfusion needs.
- Advanced design: the patch is thin and adheres firmly to the bleeding suture site, sealing it to promote faster healing. Its design creates a protective layer that keeps the stitches stable, minimizing movement and preventing displacement, which improves suture retention. The patch’s minimal thickness prevents significant swelling and avoids putting pressure on nearby tissues.
- Ease of handling: requires no rinsing before procedures, can easily be trimmed to the desired size, and accommodates cardiovascular anatomy.
- Reliable performance: improved suture retention, low thrombogenicity, and resistance to aneurysmal dilation
- Durability: non-fraying property ensures reliable performance during surgery.
Clinical evaluation
A 2023 study by Elkhouly et al. evaluated the efficacy of gelatin patch in managing sternal bleeding during cardiac surgery. Patients were divided into two groups: one with traditional methods alone, and the other with the addition of gelatin patches. Results showed that the patches significantly reduced sternal bleeding, the need for reoperation, total blood drainage, blood transfusions, and the incidence of cardiac tamponade compared to traditional methods alone. These clinical findings underscore the practical benefits of integrating gelatin patches into surgical protocols. As we conclude, it’s clear that such tools are instrumental in enhancing patient safety and recovery in cardiac surgery [2].
 Fig.1: Sternal bleeding control using gelatin patches [2].
Fig.1: Sternal bleeding control using gelatin patches [2].
Conclusion
Effective bleeding management is essential in cardiac surgery to ensure patient safety and recovery. The SURGISPON® Patch provides a reliable option for surgeons, particularly in challenging cases where traditional methods might not suffice. By supporting clot formation and reducing the risk of complications, the SURGISPON® Patch plays a significant role in improving surgical outcomes. As the needs of cardiac surgery continue to evolve, tools like the SURGISPON® Patch remain important in helping achieve successful results.
References
- Moldovan H, Antoniac I, Gheorghiță D, Safta MS, Preda S, Broască M, Badilă E, Fronea O, Scafa-Udrişte A, Cacoveanu M, Molnar A. Biomaterials as Haemostatic Agents in Cardiovascular Surgery: Review of Current Situation and Future Trends. Polymers. 2022 Mar 16;14(6):1189.
- Elkhouly M, Fouad A. The Role of Absorbable Gelatin Sponge (Gel Foam) in Control of Sternal Bleeding during Cardiac Surgery. The Egyptian Journal of Hospital Medicine. 2023 Jan 1;90(1):335-42.
- Zheng Y, Shariati K, Ghovvati M, Vo S, Origer N, Imahori T, Kaneko N, Annabi N. Hemostatic patch with ultra-strengthened mechanical properties for efficient adhesion to wet surfaces. Biomaterials. 2023 Oct 1;301:122240.
- Dunn BL, Uber WE, Ikonomidis JS. Topical thrombin preparations and their use in cardiac surgery. Open Access Surgery. 2009 Oct 23:15-34.
- Albala DM, Lawson JH. Recent clinical and investigational applications of fibrin sealant in selected surgical specialties. Journal of the American College of Surgeons. 2006 Apr 1;202(4):685-97.
- Ghavidel AA, Mirmesdagh Y, Samiei N, Dehaki MG. Haemostatic role of TachoSil surgical patch in cardiac surgery. Journal of Cardiovascular and Thoracic Research. 2014;6(2):91.
- Jarząbek R, Greberski K, Bugajski P. Autologous fibrin sealant application in cardiac surgery–a single-centre observational study. KardiochirurgiaiTorakochirurgia Polska/Polish Journal of Thoracic and Cardiovascular Surgery. 2021 Jun 1;18(2):75-9.
- Nasso G, Piancone F, Bonifazi R, Romano V, Visicchio G, De Filippo CM, Impiombato B, Fiore F, Bartolomucci F, Alessandrini F, Speziale G. Prospective, randomized clinical trial of the FloSeal matrix sealant in cardiac surgery. The Annals of thoracic surgery. 2009 Nov 1;88(5):1520-6.
- Das D, Acharya D, Singh J, Pramanik S. A detailed review of management of coronary perforations by gelfoam closure. Journal of the Practice of Cardiovascular Sciences. 2021 Sep 1;7(3):230-5.
- Cziperle DJ. Avitene™ microfibrillar collagen hemostat for adjunctive hemostasis in surgical procedures: a systematic literature review. Medical Devices: Evidence and Research. 2021 Jun 1:155-63.
- Sirlak M, Eryilmaz S, Yazicioglu L, Kiziltepe U, Eyileten Z, Durdu MS, Tasoz R, Eren NT, Aral A, Kaya B, Akalin H. Comparative study of microfibrillar collagen hemostat (Colgel) and oxidized cellulose (Surgicel) in high transfusion-risk cardiac surgery. The Journal of Thoracic and Cardiovascular Surgery. 2003 Sep 1;126(3):666-70.
- Hanks JB, Kjaergard HK, Hollingsbee DA. A comparison of the haemostatic effect of Vivostat® patient-derived fibrin sealant with oxidised cellulose (Surgicel®) in multiple surgical procedures. European Surgical Research. 2003 Oct 1;35(5):439-44.
- Bruckner BA, Blau LN, Rodriguez L, Suarez EE, Ngo UQ, Reardon MJ, Loebe M. Microporous polysaccharide hemosphere absorbable hemostat use in cardiothoracic surgical procedures. Journal of cardiothoracic surgery. 2014 Dec;9:1-7.