Unlocking Regeneration Beyond Haemostasis: Gelatin Sponges for Advanced Healing and Dermal Reconstruction in Complex Exposed Wounds

Introduction
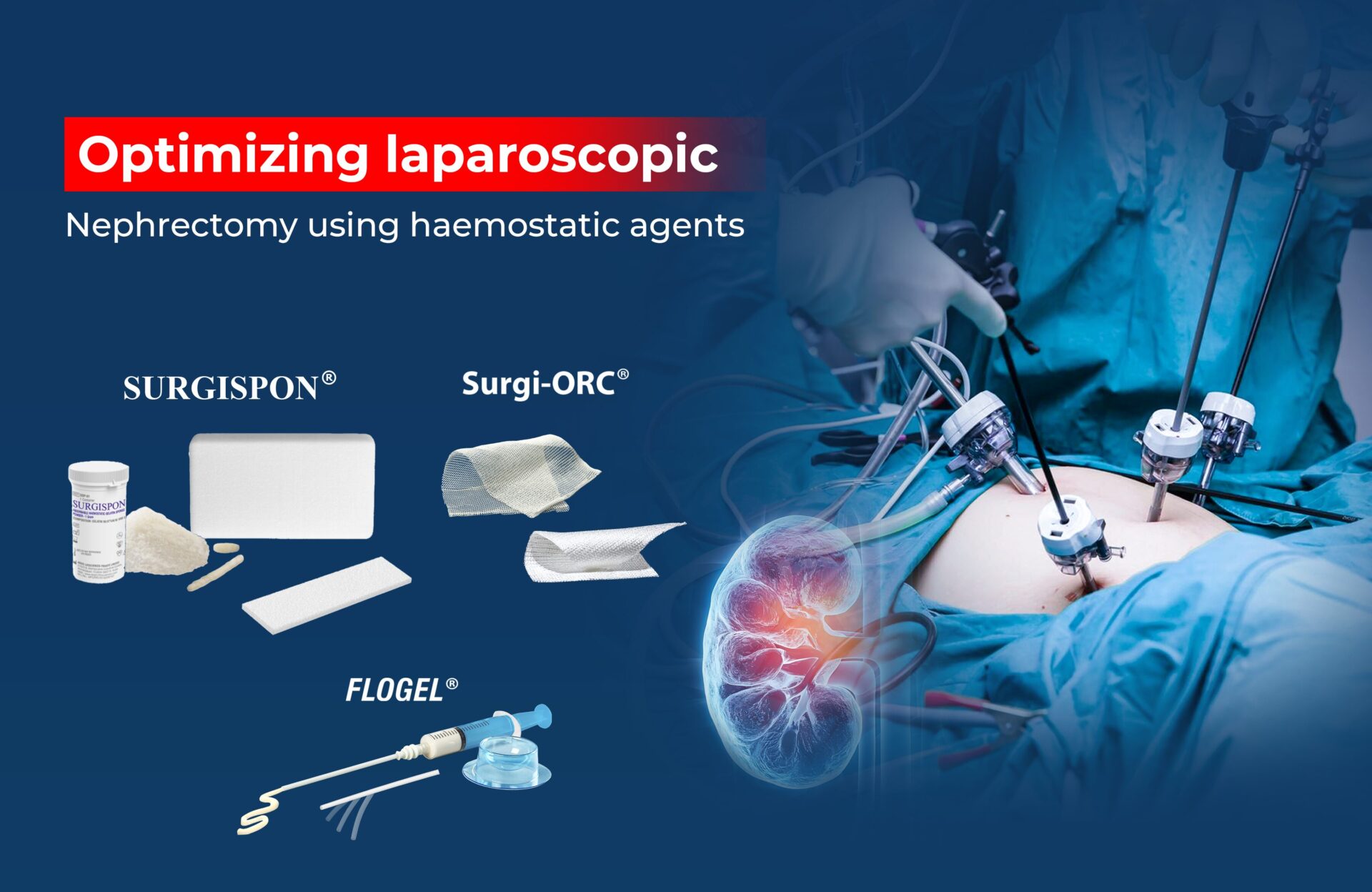
Trauma, burns, infections, or diabetic complications often result in non-healing wounds with exposed bone or tendon, posing major reconstructive challenges. These wounds require not only haemostasis but also effective dermal regeneration to restore structural integrity and prevent infection or necrosis. An Absorbable Gelatin Sponge (AGS) such as SURGISPON® offers a simple, cost-effective, and biologically compatible solution for such cases.
Beyond its well-known role in achieving haemostasis, SURGISPON® supports granulation of tissue formation, fibroblast proliferation, and epithelialization, facilitating natural dermal reconstruction.
Understanding SURGISPON® —Sterile Resorbable Haemostatic Sponge
SURGISPON® is a gamma-sterilized, non-immunogenic, and non-pyrogenic absorbable gelatin sponge that ensures rapid haemostasis and supports dermal regeneration, offering an effective solution for complex exposed wounds.
 Fig 1: SURGISPON® Sterile Resorbable Haemostatic Sponge
Fig 1: SURGISPON® Sterile Resorbable Haemostatic Sponge
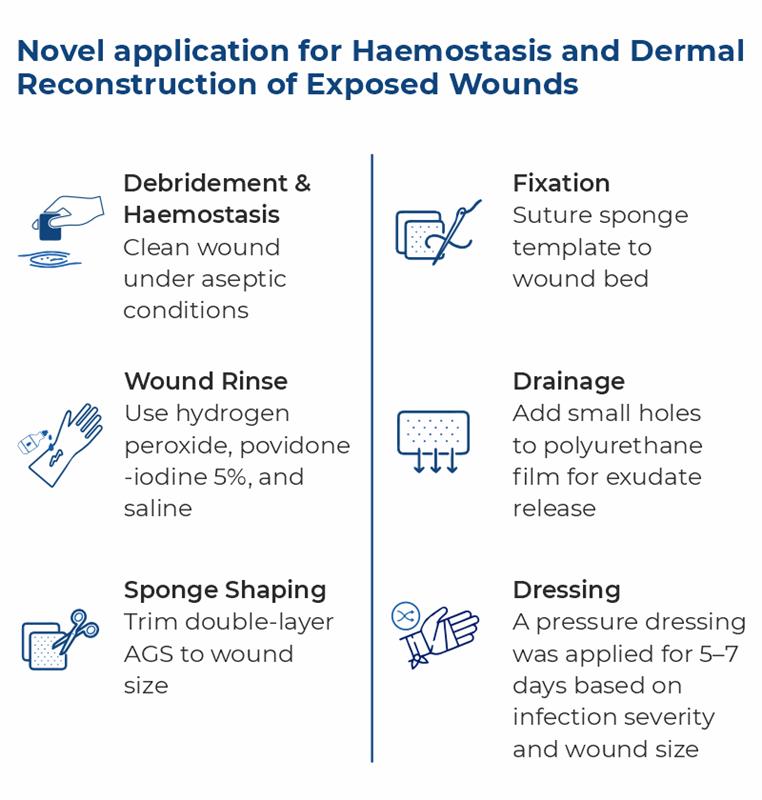
Novel application for Haemostasis and Dermal Reconstruction of Exposed Wounds
A novel clinical technique demonstrates the dual role of AGS (SURGISPON®)—for both hemostasis and dermal regeneration—when combined with polyurethane film. This combination provides an affordable alternative to advanced dermal templates like Pelnac®, making it especially valuable in resource-limited settings. The surgical steps are as follows: 1,2
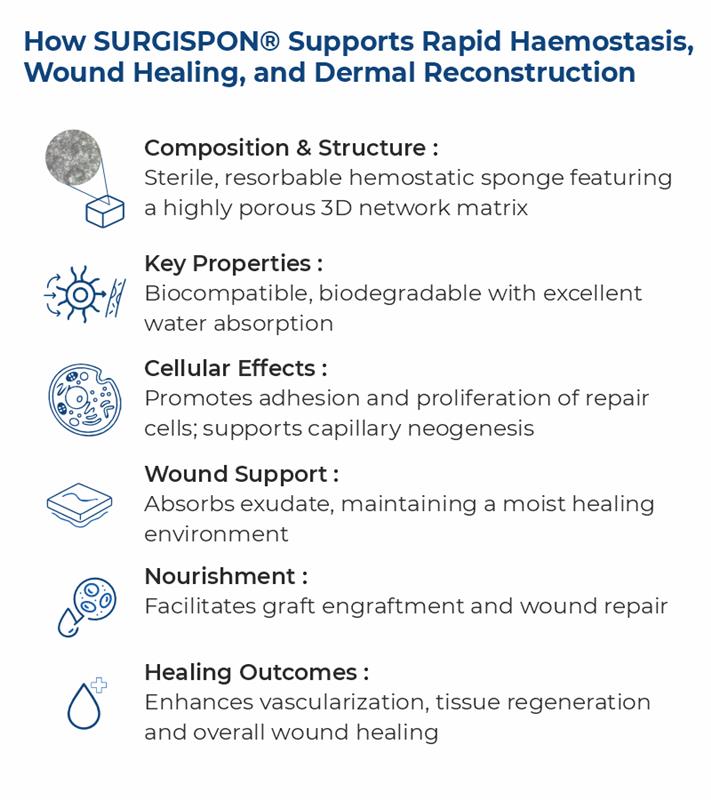
How SURGISPON® Supports Rapid Haemostasis, Wound Healing, and Dermal Reconstruction
SURGISPON® promotes adhesion and proliferation of fibroblasts, vascular endothelial cells, and epithelial cells, facilitating granulation and repair of full-thickness skin wounds.1-3
 Clinical Evidence
Clinical Evidence
Two cases of lower-extremity skin necrosis with exposed tendons were treated with early debridement, negative-pressure therapy, and saline irrigation. AGSs were applied to protect the tendons, with 0.25 mm autologous thigh mesh grafts used where granulation was insufficient. Both wounds fully healed by days 12 and 20, effectively preventing infection and necrosis.²

Fig 2: A. Necrotizing fasciitis of the left lower leg; debridement revealed exposed tendons. B. Infection control achieved with two debridements and negative-pressure wound therapy; multiple AGSs applied. C. Wound repair performed using AGSs combined with 0.25 mm autologous thigh skin grafts. D. Successful engraftment by day 12; at six months, wound showed excellent resurfacing.2
Conclusion
Absorbable gelatin sponges offer a safe, effective, and practical approach for managing complex wounds and enhancing dermal regeneration. By promoting haemostasis, supporting tissue repair, and stabilizing grafts, SURGISPON® represents an important advancement in dermal reconstruction and wound management.
References
- Yu P, Hong N, Chen M, Zou X. Novel application of absorbable gelatine sponge combined with polyurethane film for dermal reconstruction of wounds with bone or tendon exposure. International Wound Journal. 2023 Jan;20(1):18-27.
- Jing G, Wang L. Repairing Exposed Tendon Wounds with Absorbable Gelatin Sponges and Autologous Split-Thickness Skin Grafts: A Case Series. Advances in Skin & Wound Care. 2024 Jul 1;37(7):1-5.
- Jang HJ, Kim YM, Yoo BY, Seo YK. Wound-healing effects of human dermal components with gelatin dressing. Journal of biomaterials applications. 2018 Jan;32(6):716-24.