Optimizing Surgical Recovery and Haemostasis with SURGISPON® in Otologic Procedures

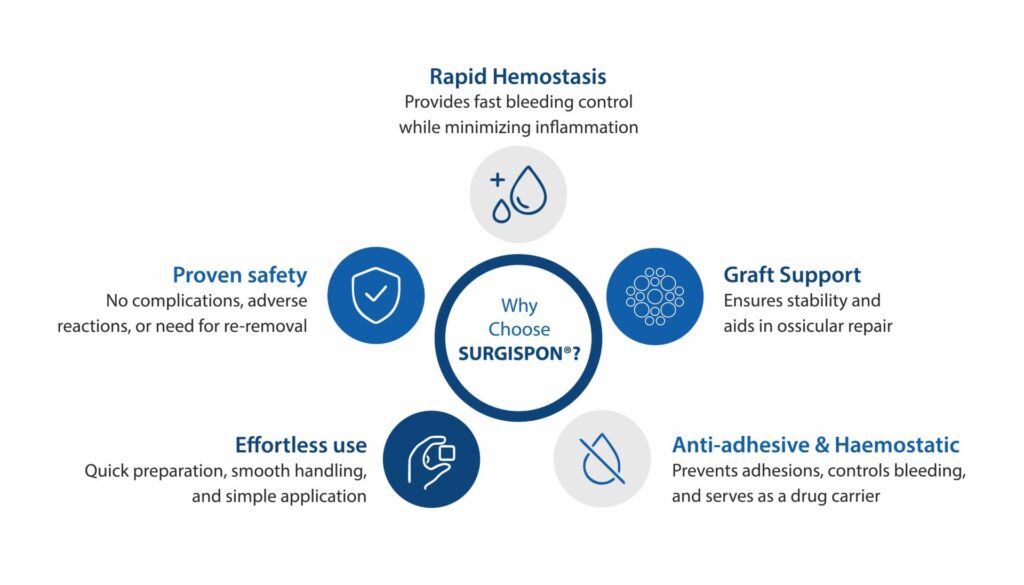
In major ear surgeries such as myringoplasty, tympanoplasty, stapedectomy, cochlear implantation, and mastoidectomy, surgeons handle some of the body’s most delicate structures. Effective haemostasis, structural support and reliable packing materials are essential to ensure surgical success and safe healing. A wide range of agents including oxidized regenerated cellulose, collagen-based products, thrombin and fibrin sealants and adhesives like cyanoacrylate or fibrin glue are commonly employed. Among these, absorbable gelatin sponges stand out by uniquely combining haemostatic action, scaffold support, and packing capability.1,2 Evidence indicates they achieve high tympanic membrane (TM) closure rates, making them a reliable first-line option for perforation repair.3
How Gelatin-Based Products Stand Out
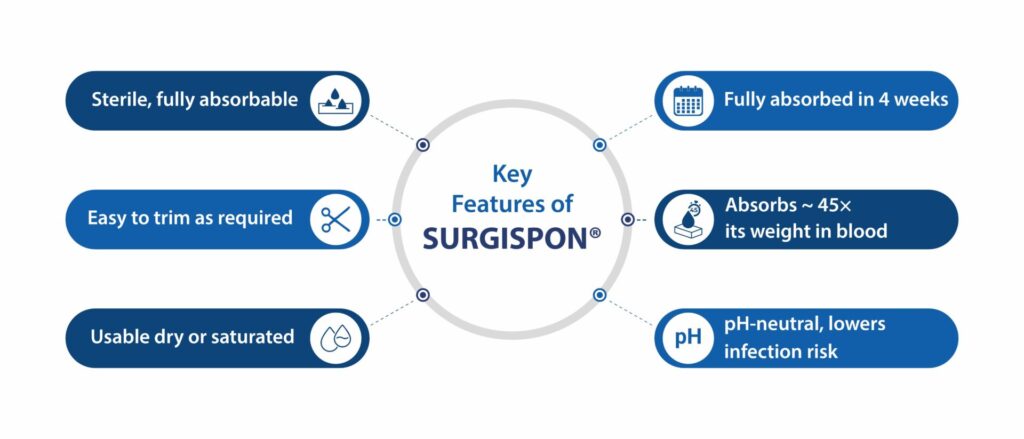
Gelatin sponges offer a unique balance of properties that make them well-suited for otologic procedures:
- Rapid haemostasis to control bleeding effectively.1
- Stable scaffold to support tympanic membrane and ossicular repair.1,3
- Cost-effective packing material that is both safe and reliable.2
Although alternatives such as hyaluronic acid, autologous fat, cartilage, fascia, and collagen have been explored, gelatin sponges remain a preferred choice due to their consistent clinical outcomes and proven safety profile.4,5
Introducing SURGISPON® – Absorbable Haemostatic Sponge
SURGISPON® is a biocompatible and surgeon-friendly gelatin sponge developed to enhance outcomes in ear surgery.
Key Features of SURGISPON®
 Why Choose SURGISPON®?
Why Choose SURGISPON®?
SURGISPON® is an absorbable sponge that offers effective and economical packing support for routine otologic procedures.
 SURGISPON® is available in multiple forms for a wide range of ear surgery applications:
SURGISPON® is available in multiple forms for a wide range of ear surgery applications:
- Standard, Cubes, Sheets, Strips and Powder

Fig. 1 SURGISPON® Absorbable Haemostatic Sponge
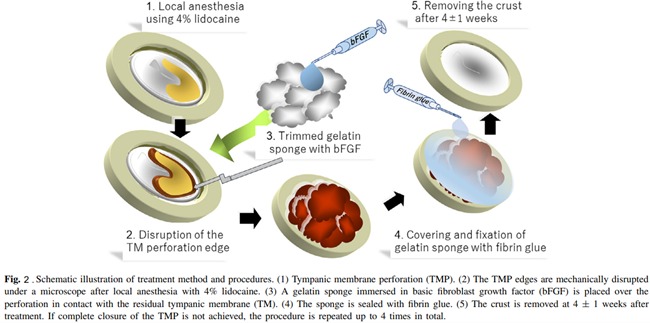
Insights from Clinical Experience on Post-Surgical Outcomes
- A multicenter, non-randomized, single-arm study of 20 patients (age 23–78; 6 males, 14 females) with chronic tympanic membrane perforation evaluated a regenerative treatment using gelatin sponge soaked in basic fibroblast growth factor and fixed with fibrin glue after mechanical edge disruption. Repeated up to four times if needed, the procedure achieved total closure in 75% of patients at 16 weeks, with a mean size reduction of 92.2% and air–bone gap improvement of 5.3 ± 4.2 dB (p < 0.0001). Thirteen patients experienced at least one adverse event, but no serious AEs occurred, supporting the treatment’s safety and effectiveness.6

Fig. 2. Schematic illustration of treatment method and procedures6
- This retrospective review of 777 myringoplasties in 604 patients (ages 1–18) at the Children’s Hospital of Pittsburgh found that successful tympanic membrane closure was significantly influenced by patient age, number and type of prior tympanostomy tubes, perforation cause, graft material, retained tubes, and Down syndrome. Gelfoam grafts achieved the highest closure rate at 90.8%, outperforming paper patch and fat grafts, highlighting the importance of choosing the right patient and graft for optimal outcomes.4
Conclusion
In ear surgery, success is shaped not only by the surgeon’s skill but also by the support of the right tools for safe healing. SURGISPON® helps make that possible by controlling bleeding effectively and protecting delicate ear structures with reliable scaffold support. It encourages smoother recovery.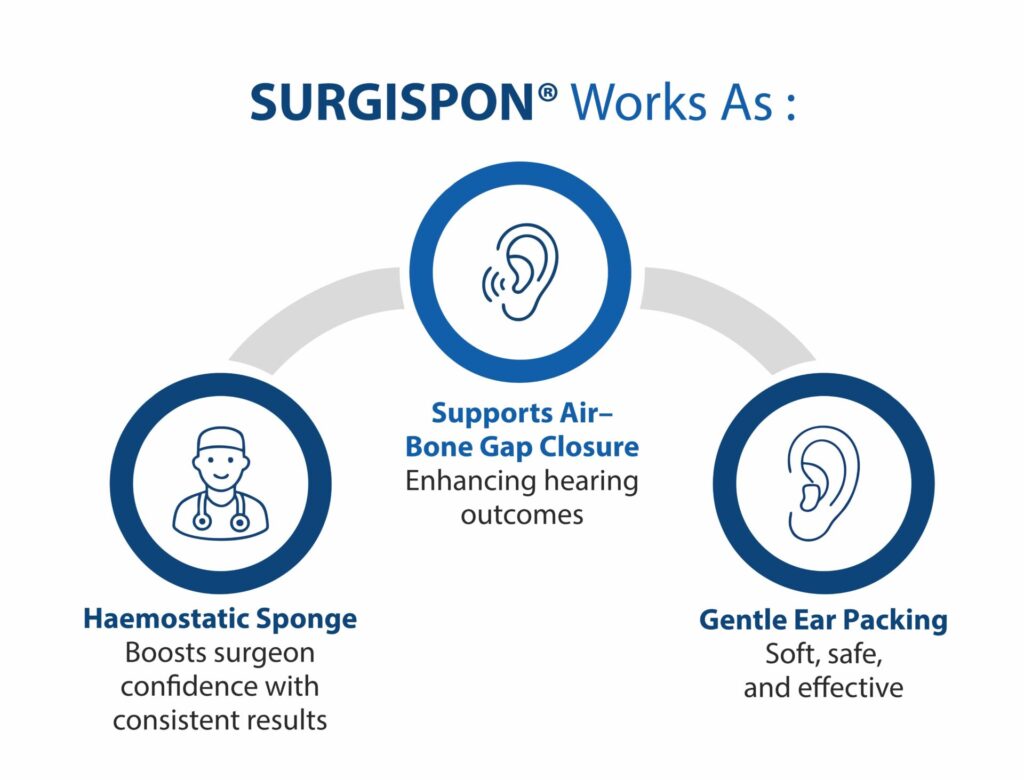
To explore more about how SURGISPON® can support safer and smoother surgical outcomes, we invite you to connect with our team or visit our product page.
References
- Li H, Roy CF, Cerruti M, Yeung JC. Structural integrity of absorbable gelatin sponges for middle ear packing in otologic surgery. Otology & Neurotology. 2023 Jun 1;44(5):e350-5.
- Fang S, Argiris K, Padgham N. How we do it: the absorbable gelatin sponge cube, an effective and economical approach to packing in ear surgery. The Journal of Laryngology & Otology. 2014 May;128(5):475-7.
- Shay EO, Shah J, Smith B, Anne S. Impact of perforation size and predictive factors for successful pediatric gelfoam myringoplasty. American Journal of Otolaryngology. 2020 Jan 1;41(1):102317.
- Sckolnick JS, Mantle B, Li J, Chi DH. Pediatric myringoplasty: factors that affect success—a retrospective study. The Laryngoscope. 2008 Apr;118(4):723-9.
- Song JS, Corsten G, Johnson LB. Evaluating short and long term outcomes following pediatric Myringoplasty with Gelfoam graft for tympanic membrane perforation following ventilation tube insertion. Journal of Otolaryngology-Head & Neck Surgery. 2019 Jan;48(1):39.
- Kanemaru SI, Kanai R, Omori K, Yamamoto N, Okano T, Kishimoto I, Ogawa K, Kanzaki S, Fujioka M, Oishi N, Naito Y. Multicenter phase III trial of regenerative treatment for chronic tympanic membrane perforation. Auris Nasus Larynx. 2021 Dec 1;48(6):1054-60.